Dysautonomia, also known as autonomic nervous system disorders, refers to a group of medical conditions causing dysfunction of the autonomic nervous system (ANS), which controls essential bodily functions such as heart rate, blood pressure, digestion, and temperature regulation. Individuals with these disorders struggle to maintain normal regulation of one or more of these systems.
More than 70 million people worldwide are affected by different types of dysautonomia.
What Are the Symptoms and Signs of Dysautonomia?
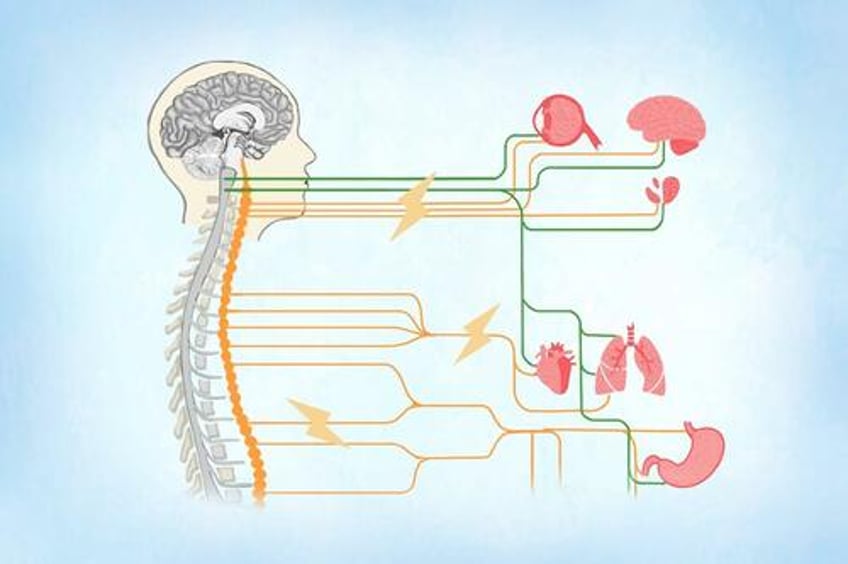
The ANS is a part of the peripheral nervous system that controls involuntary bodily functions, such as heart rate, blood pressure, digestion, respiration, and body temperature regulation. It consists of two main branches: the sympathetic nervous system and the parasympathetic nervous system.
The sympathetic nervous system is responsible for the “fight-or-flight” response by increasing heart rate, blood pressure, and energy expenditure during stress or danger.
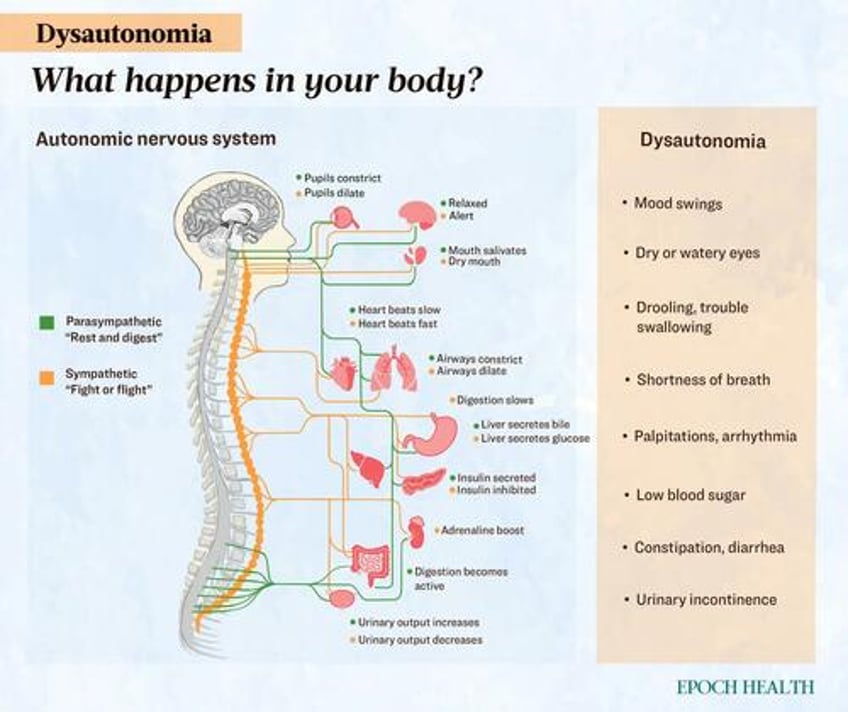
The parasympathetic nervous system is responsible for “rest-and-digest” functions by promoting relaxation, slowing the heart rate, and aiding digestion and energy conservation.
The ANS helps maintain balance (homeostasis) in the body by automatically adjusting these functions according to internal and external conditions. Dysautonomia occurs when the ANS malfunctions, causing the systems to fail to regulate the aforementioned processes properly, thus leading to various symptoms and signs.
Dysautonomia symptoms and signs can be acute and reversible or chronic and progressive. Common symptoms include those listed below.
Orthostatic Hypotension
Orthostatic (upright posture) hypotension is the most prominent symptom of dysautonomia. It results from a sudden decrease in brain blood supply when moving from a seated or supine position to standing, leading to the following symptoms:
- Dizziness
- Lightheadedness
- Fainting
- Dim or blurry vision
- Weakness
- Unsteady gait
- Slurred speech
- Exercise-induced syncope (fainting)
Urinary Dysfunction
- Increased urinary frequency
- Nocturia (the need to urinate frequently during the night)
- Urinary urgency
- Stress incontinence
Sexual Dysfunction
- Impotence
- Loss of sex drive
- Dry or retrograde ejaculation
Gastrointestinal Problems
- Intermittent diarrhea
- Explosive diarrhea (in severe cases)
- Nocturnal diarrhea
- Rectal incontinence
- Constipation
- Abdominal pain
- Acid reflux
- Heartburn
Cardiovascular Issues
- Heart palpitations
- Chest discomfort
- High or low heart rate
- High or low blood pressure
- Blood pooling, which is when blood cannot return to the heart properly and collects in the veins
Neurological Problems
- Mood swings
- Anxiety
- Forgetfulness
- Migraines
Other Symptoms and Signs
- Abnormal sweating
- Shortness of breath or difficulty breathing
- Drooling or dry mouth
- Vertigo
- Dry or watery eyes
- Trouble swallowing
- Clammy or pale skin
What Causes Dysautonomia?
Dysautonomia falls into two categories: primary and secondary. Primary dysautonomias result from genetic or degenerative diseases affecting the brain and nervous system, while secondary dysautonomias arise from injuries or other underlying conditions. The latter may be linked to medications (e.g., first-generation antipsychotics), brain trauma, or conditions such as diabetes, sarcoidosis, and certain autoimmune diseases (e.g., rheumatoid arthritis, lupus, and Sjögren’s syndrome).
Idiopathic dysautonomias are autonomic nervous system disorders with an unknown underlying cause.
Environmental factors such as medical conditions, vaccinations, and medications can cause secondary dysautonomia. Some of these include:
- Viral infections: Human immunodeficiency virus (HIV), human T-lymphotropic virus, herpes viruses, flavivirus, enterovirus 71, and lyssavirus infections can cause autonomic dysfunction.
- Lyme disease: Lyme disease can lead to the development of postural orthostatic tachycardia syndrome (POTS) and other forms of dysautonomia.
- Diabetes: Diabetes can cause diabetic autonomic neuropathy.
- Parkinson’s disease: The findings of a 2019 study indicate that autonomic dysfunction is linked to disrupted white matter, impaired brain connectivity, and cognitive decline in newly diagnosed patients with Parkinson’s disease.
- Myalgic encephalomyelitis: This is also known as chronic fatigue syndrome.
- Long COVID: A 2022 study found that symptoms of dysautonomia are common in people with long COVID. The most affected areas of dysautonomia include digestive issues, problems with sweating and other secretions, and difficulty standing up without feeling dizzy or faint. Older patients also tend to experience more orthostatic intolerance, which is when standing up causes changes such as a drop in blood pressure.
- COVID-19 vaccination: As per a 2023 study, some people experience chronic fatigue and dysautonomia after receiving the SARS-CoV-2 mRNA vaccine, a condition referred to as post-acute COVID-19 vaccination syndrome (PACVS). Researchers found that PACVS patients who had symptoms of dysautonomia for at least five months after vaccination showed different blood markers compared to healthy individuals. These differences included higher levels of certain antibodies and interleukin-6 (IL-6), which can help distinguish PACVS from a normal postvaccination response. The exact number of vaccinated individuals affected by PACVS is unknown, but current estimates suggest an incidence of about 0.02 percent.
What Are the Types of Dysautonomia?
Currently, there are at least 15 known types of dysautonomia. One individual may experience multiple types, with overlapping symptoms across them.
Ten of the more prevalent types include:
- Vasovagal syncope: Vasovagal syncope, also known as neurocardiogenic syncope, is the most common form of dysautonomia, affecting 22 percent of Americans. While many experience only occasional fainting spells, severe cases can involve fainting multiple times a day. Vasovagal syncope is a type of fainting caused by an abnormal or exaggerated response of the body’s automatic functions to stimuli such as standing up or strong emotions. The exact cause isn’t fully understood, but it involves changes in heart rate, blood pressure, and activation of specific heart fibers.
- Postural orthostatic tachycardia syndrome (POTS): POTS is characterized by an abnormally rapid increase in heart rate when moving from a sitting or lying down position to standing. It is one of the more common types of dysautonomia. Before COVID-19, POTS affected about 1 percent of teenagers and between 1 to 3 million Americans overall. Some sources suggest that this number has increased by 1 million to 3 million since the pandemic. For more details on the condition, please refer to The Essential Guide to POTS.
- Orthostatic and postprandial hypotension: Orthostatic hypotension is a sudden drop in blood pressure upon standing, leading to reduced blood flow to the brain. It often causes dizziness, lightheadedness, or fainting. Orthostatic hypotension affects approximately 6 percent of the general population and is more common in older adults, affecting 10 percent to 30 percent of this age group. Similarly, postprandial hypotension is when blood pressure drops suddenly after a meal. During digestion, the body increases blood flow to the stomach and intestines, causing the heart to pump faster and blood vessels to constrict to maintain overall blood pressure. However, in people with postprandial hypotension, the heart doesn’t speed up enough, and blood vessels fail to constrict properly, leading to a drop in blood pressure. It affects around 40 percent of older adults over 65.
- Diabetic autonomic neuropathy: Diabetic autonomic neuropathy is a common form of dysautonomia, affecting 20 percent of individuals with diabetes. It is a severe diabetes complication linked to a higher risk of cardiovascular mortality.
- Multiple system atrophy (MSA): MSA is a rare, fatal neurodegenerative disorder affecting adults over 40. It shares similarities with Parkinson’s disease but progresses more rapidly, often leaving patients bedridden within two years of diagnosis and leading to death within five to 10 years. Approximately 350,000 people worldwide are affected by MSA. Its cause is largely unknown, but the condition is associated with the deterioration and atrophy of specific brain areas, including the cerebellum, basal ganglia, and brainstem, along with the accumulation of alpha-synuclein, a protein involved in nerve cell communication.
- Familial dysautonomia: Also known as Riley-Day syndrome, familial dysautonomia is a rare inherited disorder that affects the autonomic and sensory nervous systems. It causes unstable blood pressure, reduced sensitivity to pain and temperature, and a lack of tears when crying. Individuals with familial dysautonomia may experience an autonomic crisis characterized by sudden high blood pressure, elevated heart rate, and vomiting or retching. Familial dysautonomia is caused by a genetic mutation in the ELP1 gene (also known as the IKBKAP gene), which produces a protein found in various cells, including brain cells.
- Baroreflex failure: Baroreflex failure occurs when the body’s baroreflex system, which regulates blood pressure, fails. This system sends signals to the brain to adjust blood pressure by activating the parasympathetic nervous system to lower heart rate when blood pressure is high and deactivating the sympathetic nervous system to reduce heart rate and dilate blood vessels. When blood pressure is too low, the opposite occurs. As a result of baroreflex failure, blood pressure fluctuates between being too high and too low, causing symptoms such as dizziness, fainting, headaches, sweating, and skin flushing. It is a rare condition often caused by neck trauma from surgery or radiation therapy for cancer, although in some cases, the cause is unknown.
- Pure autonomic failure (PAF): PAF, also known as Bradbury-Eggleston syndrome, is a rare form of dysautonomia characterized by the degeneration of autonomic nervous system cells. Its hallmark symptom is severe orthostatic hypotension, which leads to dizziness, fainting, and syncope. It more commonly affects men and typically occurs in middle-aged to older adults. As per estimation, fewer than 5,000 Americans live with this condition. PAF is linked to the abnormal buildup of alpha-synuclein, which is also seen in conditions such as Parkinson’s disease, MSA, and dementia with Lewy bodies.
- Inappropriate sinus tachycardia (IST): IST is a chronic condition where the heart maintains a normal rhythm but beats excessively fast, with a resting heart rate above 100 beats per minute (bpm), compared to the normal range of 60 to 100 bpm. It affects approximately 1 percent of the middle-aged population, with a higher prevalence in females. The cause of IST is unknown. One theory suggests that the sinoatrial node may have an abnormality, or the individual might be overly sensitive to adrenaline, a hormone that increases heart rate.
- Autoimmune autonomic ganglionopathy (AAG): AAG is a rare form of dysautonomia wherein the immune system attacks receptors in the autonomic ganglia, a part of the peripheral ANS. It can present with either rapid or progressive symptom onset and is often linked to high levels of ganglionic acetylcholine receptor antibodies (g-AChR antibodies). AAG affects individuals of all ages and both sexes, with about 100 cases diagnosed annually in the United States.
Who Is More Likely to Develop Dysautonomia?
The following factors put a person more at risk of certain types of dysautonomia:
- Age: POTS and vasovagal syncope is often more common among teens and young adults, causing 85 percent of fainting instances in people under 40. In people aged 50 and older, dysautonomia is usually associated with a neurodegenerative disease.
- Sex: POTS is most commonly observed in women of childbearing age, typically between 15 and 50 years old.
- Ethnicity: People of Ashkenazi Jewish descent are at a higher risk of dysautonomia, especially familial dysautonomia, which affects almost exclusively this population.
- Diabetes: Diabetics are prone to developing diabetic autonomic neuropathy.
- Alcoholism: Excessive drinking is known to affect the ANS.
- Injury or surgery: An event that damages the ANS or brain can lead to dysautonomia.
- Vitamin deficiencies: Examples include vitamin B12 and vitamin D deficiencies.
- Deconditioning: Deconditioning is the loss of physical function due to lack of activity, extended bed rest, or a very sedentary lifestyle.
- Certain medical conditions: These conditions include amyloidosis, celiac disease, mitochondrial diseases, mast cell disorders, complex regional pain syndrome (CRPS), various autoimmune diseases, and Sjögren’s syndrome.
Read the rest here...

