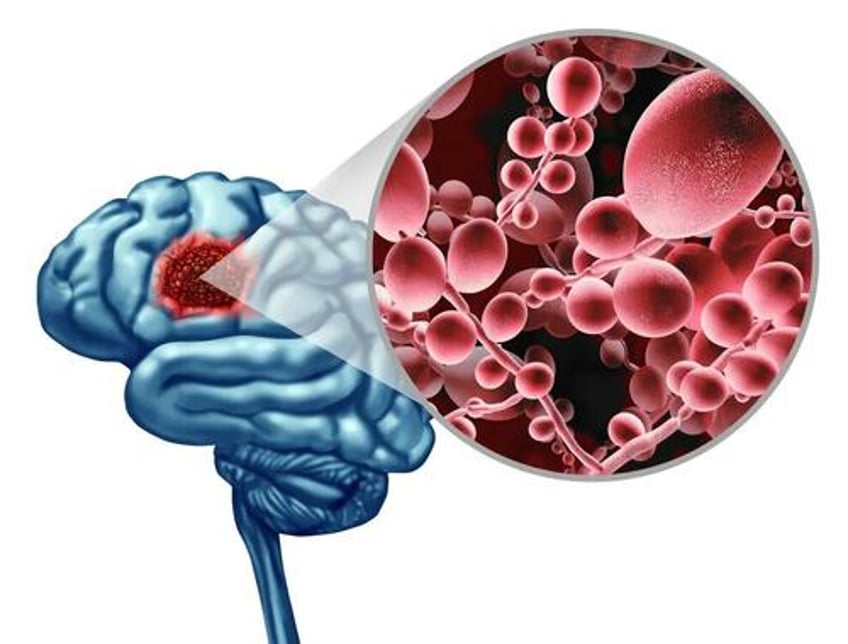
A team of researchers at Baylor College of Medicine has discovered that when the brain is infected with a common fungus, it changes in ways similar to those seen in Alzheimer’s disease. The new research delves deeper into some of the molecular mechanisms behind that process.
The Study Findings
Using animal models, the research team discovered how the fungus, called Candida albicans (C. albicans), enters the brain, activates mechanisms for its clearance, and generates amyloid beta (Aβ)-like peptides—toxic protein fragments thought to be central to the development of Alzheimer’s disease.
Previous research has implicated fungi in the development of chronic neurodegenerative diseases like Alzheimer’s disease, but their mechanisms are not entirely understood.
A Microbial Cause of Alzheimer's?
A separate review published in the journal NeuroSci in 2022 explored the question of whether dementia has a microbial cause. The report concluded that the reviewed data suggests infectious agents, like fungi, can play a role in the process through which Alzheimer’s disease and other forms of dementia develop.
“Our lab has years of experience studying fungi, so we embarked on the study of the connection between C. albicans and Alzheimer’s disease in animal models,” said Dr. David Corry, one of the study’s authors and a professor of pathology and immunology and medicine at Baylor College in a news release on Oct. 17. “In 2019, we reported that C. albicans does get into the brain, where it produces changes that are very similar to what is seen in Alzheimer’s disease. The current study extends that work to understand the molecular mechanisms.”
“Our first question was, how does C. albicans enter the brain? We found that C. albicans produces enzymes called secreted aspartic proteases (Saps) that breakdown the blood-brain barrier, giving the fungus access to the brain where it causes damage,” Yifan Wu, the study's lead author and a postdoctoral scientist in pediatrics said in a press release.
The researchers’ next goal was to determine how the brain was able to clear the fungal infection. Dr. Corry and his colleagues had done previous research that showed an infection in the brain by C. albicans can be completely healed in ten days in healthy mice. Those findings, published in Nature Communications in January 2019 found that the fungal infection was cleared due to two mechanisms that were triggered by the fungus in specific brain cells called microglia.
Microglia are a type of glial cell located throughout the brain and spinal cord and represent approximately 10–15 percent of the cells found in the brain. Microglia act as a primary line of immune system defense and scavenge the central nervous system for pathogenic organisms, damaged neurons, and other foreign material so they can be destroyed through a process called phagocytosis.
In the present study, the researchers demonstrated that Aβ-like peptides can be created by C. albicans. Candida albicans is a common fungus and has been found in the brains of people with Alzheimer’s disease as well as in those with other chronic neurodegenerative disorders.
What is Candida Albicans
Candida albicans is a common fungus (in the form of yeast) and is present in the gastrointestinal tract, the mouth, the skin, and the reproductive tract of most humans.
Humans and C. albicans have a complicated relationship, as most of the time, C. albicans is harmless and is simply a member of a healthy microbiota. However, it is one of the few fungal species that cause disease in humans and is responsible for infections that range from superficial infections of the mucosa and skin, like thrush, diaper rash, and vaginal yeast infections, to more serious infections like invasive candidiasis that can affect the blood, heart, brain, and bones.
Infections by C. albicans are particularly dangerous for those with compromised immune systems, like those with AIDS, or people undergoing immunosuppressive therapies for cancer and other conditions. This suppression of the body’s defenses is part of the reason why some people acquire C. albicans infections after taking antibiotics, as they decrease the beneficial bacteria in the gut, causing an imbalance and allowing C. albicans to thrive. C. Albicans can survive outside the body and have the ability to colonize every human organ and tissue. According to the Encyclopedia of Microbiology, it is the most common cause of systemic fungal infections.
More Evidence Linking Fungi to Neurodegenerative Diseases
In a January review published in Frontiers in Immunology, researchers examined the role of fungus in central nervous system autoimmune and neurodegenerative disorders. The review states that recently, increasing evidence has pointed to the role of peripheral fungus in triggering inflammation, immune response, and worsening of a range of non-infectious disorders of the central nervous system (CNS), including multiple sclerosis, Parkinson’s, and Alzheimer’s disease.
The review concluded that fungus can trigger inflammation via different mechanisms in the progression of CNS non-infectious diseases, suggesting that it is crucial for developing future therapeutic agents and strategies.
A 2015 study published in Scientific Reports states that several researchers have proposed the possibility that Alzheimer’s disease may have a microbial cause. The researchers found evidence that tissue from the central nervous system (which includes the brain and spinal cord) of patients with Alzheimer’s disease contains fungal cells. These fungal cells were found in different regions of the brain, including the external frontal cortex, cerebellar hemisphere, entorhinal cortex/hippocampus, and choroid plexus. These fungal materials were not present in the control individuals who did not have Alzheimer’s disease. The researchers identified several different species of fungus in their samples.
Interestingly, the study authors noted that fungal infection was also found in the blood vessels, which could explain the vascular pathology that is often found in Alzheimer’s patients.
The findings provide intriguing evidence that these fungal infections are present in the central nervous systems of those with Alzheimer’s disease and not in healthy individuals who served as the controls.
Another Piece of the Puzzle
Dr. Corry and his colleagues have provided another piece to further understand the role fungus may play in the development of Alzheimer’s disease.
“This work potentially contributes an important new piece of the puzzle regarding the development of Alzheimer’s disease,” Corry said in a press release. “The current explanation for this condition is that it is mostly the result of the accumulation of toxic Aβ-like peptides in the brain that leads to neurodegeneration. The dominant thinking is that these peptides are produced endogenously [internally], our own brain proteases break down the amyloid precursor proteins generating the toxic Ab peptides.”
However, in their study, the researchers show that these Aβ-like peptides can also be created from another source–candida albicans.
“These findings in animal models support conducting further studies to evaluate the role of C. albicans in the development of Alzheimer’s disease in people, which can potentially lead to innovative therapeutic strategies.” Dr. Corry said.
