Between 2013 and 2021, rates of immunosuppression in adults have doubled, according to estimates from a Journal of the American Medical Association (JAMA) research letter.
In 2021, an estimated 6.6 percent of U.S. adults were immunosuppressed. “This rate of immunosuppression was higher than the previous national estimate of 2.7 percent using the 2013 [National Health Interview Survey],” the authors wrote in their paper.
The researchers estimated immunosuppression prevalence by analyzing National Health Interview Survey (NHIS) results.
Specifically, the authors analyzed responses to five questions. Over 29,000 individuals were asked if they had a health condition or were taking medication or treatments that would weaken their immune system. They were also asked if they had cancer or malignancy, the type of cancer, and their age at the time of cancer diagnosis.
In 2013, over 34,000 people were interviewed, garnering a response from 75 percent of households. In 2021, only about half of the households contacted responded to the survey.
Why the Rise in Immunosuppression?
“Given the documented increase in immunosuppression, studies are needed to understand the causes for this increase,” the authors wrote. However, they mentioned that the rise in self-reported immunosuppression may be due to increased use of immunosuppressive medications.
The use of adalimumab, a drug used to treat autoimmune conditions, has increased 3.5-fold between 2014 and 2021.
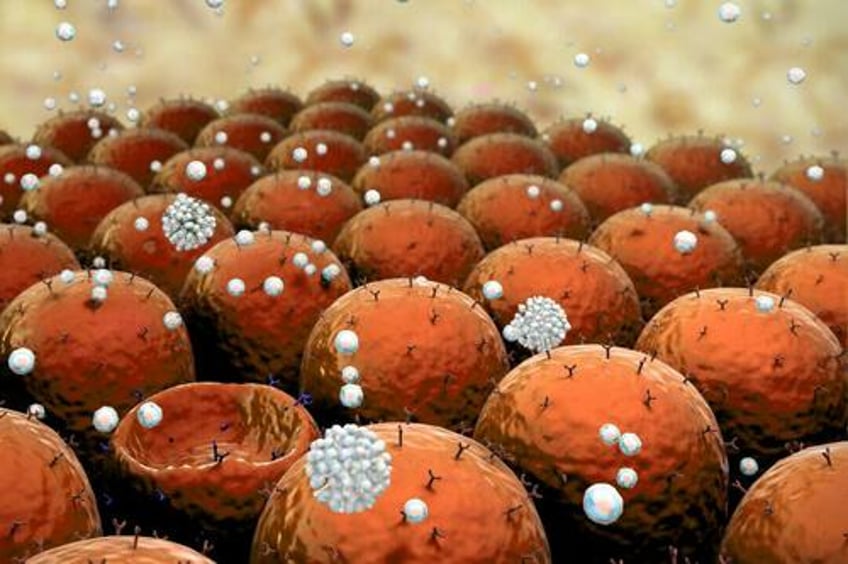
Immunosuppression carries significant risks, “including an increased susceptibility to infections, potential organ rejection, side effects of immunosuppressant drugs, elevated cancer risk, and pregnancy-related concerns,” Mohammad Razzaque, professor of pathology at the Lake Erie College of Osteopathic Medicine, told The Epoch Times.
Immunosuppression occurs naturally with age, but it can also occur due to the individual being on various immunosuppressive therapies. People undergoing such therapies include organ transplant patients and those with autoimmune diseases or cancer.
Dr. William Schaffner, a professor of medicine and preventative medicine at the Vanderbilt University School of Medicine, reasoned that the rising prevalence could signify progress in science and health.
“There are more and more people being kept alive and are being treated with immunosuppressant agents in the United States, and that treatment is extending life, which means that the proportion of the population that is immunosuppressed is increasing,” Dr. Schaffner said.
Crude data from NHIS have also shown a rise in self-reported rates of cancer. According to 2015 U.S. Centers for Disease Control and Prevention (CDC) statistics, 8.7 percent of adults reported cancer. In 2021, it was estimated that 9.8 percent of adults had cancer.
NHIS' most recent survey in 2022 estimated that a slight decrease of 9.6 percent of adults had cancer.
The COVID-19 pandemic may have also made individuals more aware of their immune health and whether they are immunosuppressed, the research letter authors added.
COVID-19 and Immunosuppression
Studies have shown that the COVID-19 virus can disrupt the function and order of the immune system, leading to immune dysfunction and possible immunodeficiency.
One 2o23 study published in Nature Reviews Rheumatology found that people with a COVID-19 infection are at a greater risk of developing autoimmune diseases, which may be linked to potential immunodeficiencies.
The COVID-19 pandemic may have been particularly challenging to those already immunocompromised.
Immunocompromised people tend to have an increased disease severity if they become infected with COVID-19, and the vaccine appears to be less effective for them. Public health measures put in place during the pandemic may also have created obstacles for these people to access health care and therapies for their immunosuppression, said Mr. Razzaque.
Other researchers and physicians argue that the COVID-19 vaccines may also contribute to immunosuppression and deficiencies, though some research has opposite findings.
Research from Cleveland Clinic suggests that repeated boosting of COVID-19 vaccinations has been shown to put a person at risk of future COVID-19 infections. Another letter to the editor from Columbia University authors published in the New England Journal of Medicine showed that people with higher vaccine antibody levels after vaccination were more strongly associated with breakthrough infections.
Most recently, an Australian review suggested that repeat COVID-19 vaccine boosting in immunocompromised individuals may impair immune activation within this population, possibly making them more vulnerable to infections and cancers.
In a research paper, Mr. Razzaque pointed to increased influenza infections reported in people who receive repeat influenza vaccinations, speculating if frequent boosting may be linked to immunosuppression.
Dr. Schaffner said whether increased infections linked to repeat vaccinations are a sign of general immunosuppression is debatable.
“It’s a very debatable issue,” he said, adding that even if there is an increased risk of COVID-19 infection linked to repeat vaccination, there does not seem to be “serious evidence” indicating a “general suppression of the immune system.”
However, works by Nordic researchers Drs. Peter Aaby and Christine Stabell Benn suggest that non-live vaccines, including COVID-19 and influenza vaccines, tend to make the immune system “lazy” and less equipped to fight an infection. In contrast, live vaccines train the immune system to become better fighters.
Gastroenterologist and CEO of ProgenaBiome, Dr. Sabine Hazan, has said that the COVID-19 vaccine may cause immunosuppression by reducing good Bifidobacteria in the gut. She showed that after COVID-19 mRNA vaccination, Bifidobacteria levels dropped by half among her trial participants.
Bifidobacteria are essential for boosting intestinal immunity. Dr. Hazan’s earlier work showed that people with reduced Bifidobacteria in the gut were at risk of severe COVID-19 infections, and therapeutics that replenished the Bifidobacteria, such as vitamins C and D and ivermectin improved patient survival rates.
“The pandemic appears to have influenced what the public thinks about their immune system. There has been a big jump in perceived weakness in the immune system. More research is needed to determine if either SARS-CoV-2 infection or COVID-19 vaccine indeed has impaired human immunity according to these perceptions,” Dr. Peter McCullough, renowned cardiologist and internist, told The Epoch Times.
