CAR T-cell therapy turns patient's cells into a cancer-fighting weapon: ‘Extremely high response rates’
When it comes to cancer treatments, most people are familiar with chemotherapy, radiation and surgery.
Yet there is another emerging, lesser-known therapy that is showing promising results in treating blood cancers.
With CAR T-cell therapy, the patient’s T-cells are taken from the blood, engineered to attack cancer cells and then infused back into the patient’s body through an IV, Dr. Noopur Raje told Fox News Digital.
Raje is director of the Center for Multiple Myeloma at Massachusetts General Hospital, which has a Gene and Cell Therapy Institute that offers CAR T-cell therapy.
JUST 4 MINUTES OF INTENSE DAILY ACTIVITY COULD SLASH CANCER RISK AMONG ‘NON-EXERCISERS,’ STUDY FINDS
"I think it's made a big change in people's lives and how we take care of people," she told Fox News Digital in an interview.
"It's one of the most personalized ways of taking care of some of the blood-related cancers."

Dr. Noopur Raje is director of the Center for Multiple Myeloma at Massachusetts General Hospital, which has a Gene and Cell Therapy Institute that offers CAR T-cell therapy. "It's one of the most personalized ways of taking care of some of the blood-related cancers," she said of the therapy. (Mass General Cancer Center)
At Mass General, Raje and her team treat patients with multiple myeloma, a rare form of blood cancer that attacks the plasma cells.
Most of their patients are between 60 and 70 years old, she said.
What is CAR T-cell therapy?
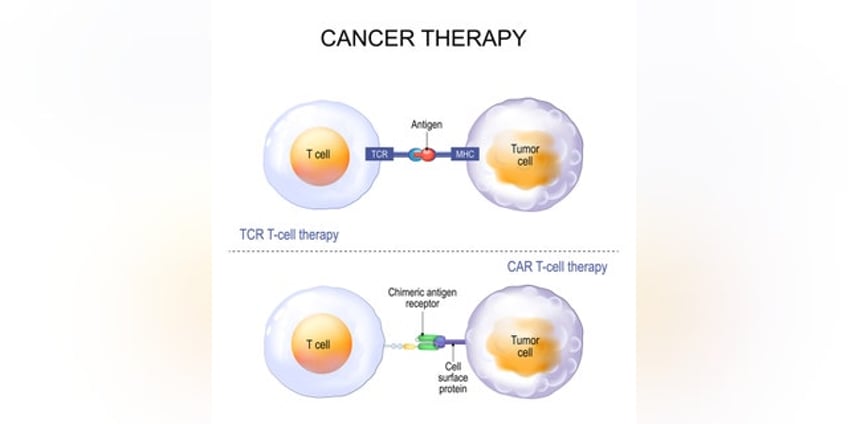
CAR stands for chimeric antigen receptors, which are proteins that enable T-cells to target the tumor antigens produced by cancer cells.
T-cells are a type of white blood cell that helps to fight germs and prevent disease, per the Cleveland Clinic.
There are currently six CAR T-cell therapies that are FDA-approved to treat leukemia, lymphomas, multiple myeloma and other blood cancers.

As of now, the FDA has approved CAR T-cell therapy as a "last resort" when the disease has persisted through all other available treatments. (iStock)
"We are taking our patients’ T-cells, which are the immune cells, and then activating them and putting a chimeric antigen receptor (CAR), which can recognize a protein on a cancer tumor," Raje said.
CANCER BLOOD TEST USING DNA FRAGMENTS BRINGS HOPE FOR EARLIER DETECTION, SAY RESEARCHERS
Because Raje treats multiple myeloma, her team started off by doing studies against a protein called BCMA, which is found in cancerous plasma cells.
The re-engineered T-cells continue multiplying in the body, so they can seek out and kill more tumor cells, the doctor said.
With CAR T-cell therapy, the patient’s T-cells are taken from the blood, engineered to attack cancer cells and then infused back into the patient’s body through an IV. (iStock)
"We are seeing extremely high response rates, between 82% and 100%," she told Fox News Digital. "Now we need to do a better job of maintaining that response."
Before CAR T-cell therapy, Raje said, patients were started on a treatment and then stayed on it for an indefinite length of time.
"This is the first time that patients are getting a ‘one-off’ treatment, and then we're just watching them with no more treatment at all," she said.
Once the process is complete, the patient receives no new therapies for up to three years.
While the treatment can be a little "involved" at the beginning, Raje said, once it’s complete the patient receives no new therapies for up to three years.
"And I have some patients who are on no treatment for way longer than that, which is a big advancement," she added.
"Obviously, we need to do better — we need to cure people," Raje said.
"We're not quite there, but the next step is to start the treatment earlier, so we can start seeing more control of the disease over a longer period of time."

Sandy Caterine is pictured leaving the hospital after receiving CAR T-cell therapy in 2019. (Sandy Caterine)
As of now, the FDA has approved CAR T-cell therapy as a "last resort" when the disease has persisted through all other available treatments; but Raje hopes that soon, it will be available to patients earlier in the course of their cancers.
CAR T-cell therapy is expensive — costing anywhere from $500,000 to $1,000,000, per WebMD. Raje pointed out, however, that many insurance plans cover at least some of the cost. It is also covered by Medicare.
"I think one has to start looking at the time saved in terms of quality of life in not coming back to the hospital and not being on any other meds," she said.
AI TECH AIMS TO DETECT BREAST CANCER BY MIMICKING RADIOLOGISTS’ EYE MOVEMENTS: 'A CRITICAL FRIEND'
There is some risk of side effects for those receiving CAR T-cell therapy, primarily a condition called cytokine release syndrome (CRS). It can occur when the immune system responds too aggressively to infection.
"When the CAR T-cell kills the tumor, it produces a bunch of proteins, and when it does that, it can make you quite sick," Raje said.

Sandy Caterine of New Hampshire (center in green dress) is pictured with her extended family in June 2021 after her successful CAR T-cell therapy. (Sandy Caterine)
"But as we've used more and more of these therapies, we've gotten pretty good at managing this, and we have the antidotes for these kinds of toxicities," she added.
Another potential side effect is a condition called ICANS, or immune effector-mediated neurotoxicity.
"With this, people can get confused, sometimes to the extent that they can actually go into a deep coma," Raje said. "It's important to recognize and treat these conditions earlier."
One woman's story: ‘A great response’
Sandy Caterine, a retired accountant who lives in Rye, New Hampshire, was part of a clinical trial for CAR T-cell therapy.
She was diagnosed with multiple myeloma in August 2019.
"It kind of came out of nowhere," Caterine told Fox News Digital. "In retrospect, maybe I had a couple of little symptoms."
Caterine had experienced some back pain, fatigue and nausea, but initially chalked it up to dehydration.
When the symptoms didn’t go away on their own, she saw her primary care physician and got some blood tests, which led to her diagnosis.

Sandy Caterine is pictured visiting her grandson in New Orleans in 2023. (Sandy Caterine)
"I had never even heard of multiple myeloma," Caterine said. "All I heard was that it was incurable and no one could predict what the life expectancy might be."
For several months, Caterine was on a regimen of numerous drugs, infusions and radiation, none of which fully resolved her cancer. Then she learned about the clinical trial for CAR T-cell therapy.
"Sandy has what is known as high-risk disease, based on the genetics of the cancer," said Raje. "This usually doesn’t have good outcomes, but Sandy had a great response to the trial."
Caterine, who is 62, did experience the CRS illness as a side effect, which caused her to endure nausea, fatigue, fever and disorientation.
She remained in the hospital for 15 days.
"It took me a while to get my strength back," she said. "I do remember them taking very good care of me."
Caterine has gotten periodic bone marrow scans every three months since her infusion.

Sandy Caterine (center, right, near Mickey's ear) is pictured in February 2023 with her daughter, her sister and her family. (Sandy Caterine)
"So far, there has been no sign of the disease," she said.
"Dr. Raje told me the hope was that it would work for two to three years, and I am already over two years."
Caterine’s experience has helped her appreciate each day more than she did before, she told Fox News Digital.
"It's probably the most personalized way of being able to take care of your own disease."
"These are two years that I never thought I would get when I was first diagnosed," she said.
"It's just great that I can continue to live my life and be with my family."
Future of CAR T-cell therapy
CAR T-cell therapy started out for use in leukemia, later branching out to other blood cancers like lymphoma and multiple myeloma.
Raje is hopeful that the treatment eventually will become available for other types of cancers, including cancers of the breast, colon and brain.
CLICK HERE TO SIGN UP FOR OUR HEALTH NEWSLETTER
"We have an ongoing study where we are looking at CAR T-cell therapy in glioblastoma, a type of brain cancer, which we would have never thought of doing early on," she said.
"And we have a whole host of new CARs coming down the pike against different antigens."
"Obviously, we need to do better — we need to cure people."
The doctor emphasized the significance of teaching the body’s own immune cells to fight against cancer cells.
"In my mind, it's probably the most personalized way of being able to take care of your own disease, which is amazing," she said.
Melissa Rudy is health editor and a member of the lifestyle team at Fox News Digital.
