Peripheral neuropathy (PN) is a severe and complex neurological disorder affecting 20 million to 30 million people in the United States.
PN damages nerves outside the brain and spinal cord, primarily in the feet and hands. Symptoms such as numbness, tingling, burning pain, and muscle weakness can drastically reduce quality of life, making even simple tasks challenging.
Identifying and treating the root cause of PN is vital to prevent further nerve damage and preserve mobility. If left unaddressed, PN can lead to severe complications, including the risk of limb amputation.
What Are the Symptoms and Early Signs of Peripheral Neuropathy?
Recognizing the symptoms of PN is necessary for early diagnosis and treatment to prevent irreversible damage. Common early warning signs include numbness that may feel like “walking on pillows” and pain or burning sensations in the feet or hands.
PN can manifest differently depending on the cause and the type of nerves affected. Symptoms vary widely; some individuals experience severe pain, while others might have numbness with little discomfort. The onset can be gradual, as seen in diabetic peripheral neuropathy (DPN), or sudden, as in neuropathy from toxic exposure or Guillain-Barré syndrome.
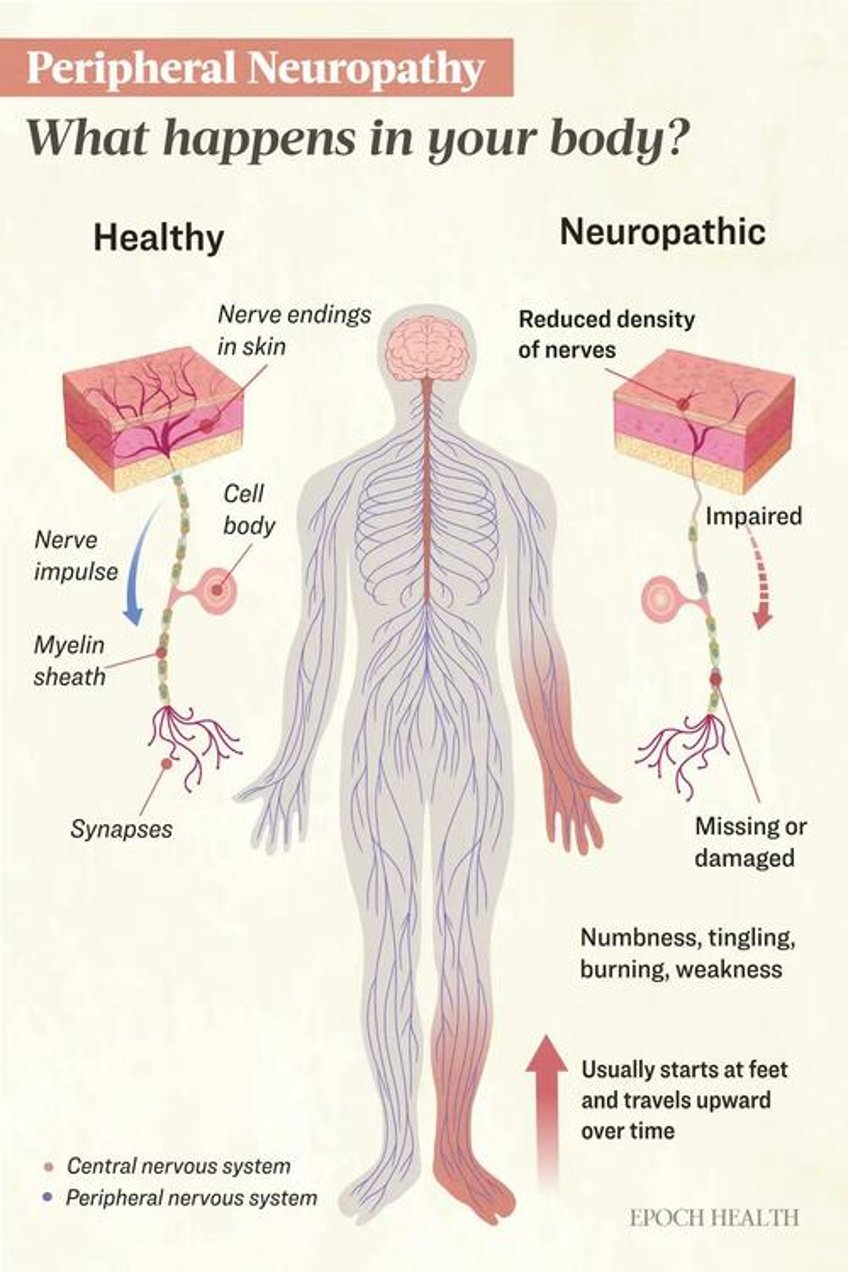
Typically, PN follows a “stocking and glove” pattern, starting at the feet and progressing upward, eventually affecting the hands. This pattern occurs because the longest nerves are most susceptible to damage due to issues like reduced blood flow and metabolic disturbances.
Peripheral nerves consist of sensory, motor, and autonomic nerves, with symptoms varying based on which type is affected. The severity and progression of symptoms also depend on whether the nerves are myelinated (with a protective sheath) or unmyelinated. Damage can be axonal or demyelinating, affecting the nerve fibers or the myelin sheath, respectively.
Sensory Nerves
These nerves transmit sensations like touch, temperature, and pain. Many sensory nerves, especially pain-sensing fibers, are unmyelinated and may be affected more gradually. Damage can cause:
- A tingling feeling, often described as “pins and needles”
- Numbness or a complete loss of feeling
- Increased sensitivity to touch or pain (hyperesthesia) and pain from things that usually do not hurt (allodynia)
- Problems with balance or walking due to loss of body awareness (sensory ataxia)
- Deep aching sensations
- Tiredness after activity
- Itching that feels different from regular itching (neuropathic itch)
Motor Nerves
These nerves control muscle movement. Most motor nerves are myelinated, allowing faster signal conduction and potentially quicker symptom onset when damaged. When affected, symptoms may include:
- Muscle weakness
- Difficulty with fine motor skills, like buttoning a shirt
- Trouble walking or maintaining balance
Autonomic Nerves
These nerves regulate involuntary functions and may be myelinated or unmyelinated. Symptoms include:
- Feeling dizzy when standing up
- Slow digestion (gastroparesis)
- Constipation or diarrhea
- Bladder problems
- Sexual dysfunction
- Blurry vision
- Dry eyes, mouth, or skin
- Burning and flushing of the skin
What Causes Peripheral Neuropathy?
PN is not a single condition but rather a group of related disorders that can have various causes and symptoms. PN occurs when the peripheral nerves, which connect the brain and spinal cord to the rest of the body, are damaged. This damage can occur through various metabolic and cellular pathways, affecting the nerves in different ways but ultimately leading to disruptions in nerve function. The development is often complex and likely involves multiple contributing factors.
The following list of mechanisms and causes is not exhaustive, and ongoing research continues to uncover new insights, but some of the leading causes include the following:
- Metabolic factors: In conditions like Type 2 diabetes and metabolic syndrome, high blood sugar and lipid levels can disrupt nerve function and decrease blood flow to the nerves. In Type 1 diabetes, the deficiency of insulin and C-peptide, rather than excess glucose alone, may contribute to nerve damage. Ironically, rapid reductions in blood glucose levels during treatment can lead to treatment-induced neuropathy.
- Mitochondrial dysfunction: The energy-producing structures within cells, called mitochondria, can malfunction, resulting in reduced energy production and increased harmful reactive oxygen species (ROS). While ROS play important roles in cellular signaling, an excess can harm nerve cells.
- Protein misfolding: Misfolded proteins, such as amyloid, can impair blood supply, trigger inflammation, and cause toxicity to nerve cells.
- Circulatory problems: Reduced blood flow from conditions like peripheral artery disease limits oxygen and nutrients to nerves.
- Immune-mediated and autoimmune causes: Conditions like Guillain-Barré syndrome and lupus involve the immune system attacking nerves. Paraneoplastic neuropathy occurs when the immune response to cancer targets healthy nerves. Other autoimmune diseases, such as Sjogren’s syndrome, vasculitis, Crohn’s disease, ulcerative colitis, sarcoidosis, rheumatoid arthritis, and psoriatic arthritis, cause nerve damage indirectly. This can occur through chronic inflammation, nerve compression, nutrient malabsorption, blood vessel inflammation or damage, or granulomas that compress nerves or disrupt their blood supply.
- Gluten-related sensitivities: Celiac disease and non-celiac gluten sensitivity may cause nerve damage through inflammation or malabsorption. Notably, one study found that 34 percent of people with idiopathic (unexplained) neuropathy had evidence of gluten sensitivity, and 9 percent had biopsy-confirmed celiac disease.
- Physical trauma: Injuries or pressure on nerves occurring alongside conditions like carpal tunnel syndrome, tumors, and compression injuries can lead to damage.
- Infections and vaccine reactions: Infections from certain viruses or bacteria, such as human immunodeficiency virus (HIV), hepatitis C, Lyme disease, shingles, COVID-19, and Campylobacter jejuni, can directly attack nerve tissue or trigger immune responses that damage nerves. PN has also been reported after vaccination for COVID-19, shingles, tetanus-diphtheria-pertussis (Tdap), and influenza.
- Toxic exposures: Chemicals, medications, and environmental toxins can damage nerves. Many medications, including certain chemotherapy drugs, antibiotics, and cardiovascular and antiviral medications, can affect nerves. Other toxic exposures include heavy metals, solvents, pesticides, industrial chemicals, and chronic alcohol use.
- Hereditary disorders: Genetic conditions, like Charcot-Marie-Tooth disease (CMT), affect nerve development and function. CMT often leads to muscle weakness and wasting in the lower legs and feet, causing high arches, hammer toes, and skin discoloration. In severe cases, hand muscles can also waste away, making the fingers curl into a “claw” shape.
- Nutritional deficiencies: Deficiencies in vitamins D, B1 (thiamine), B12, and E, as well as copper and folate, can lead to PN. Malabsorption, chronic alcohol use, and bariatric surgery worsen these deficiencies. Conversely, excessive vitamin B6 intake can cause neuropathy.
- Chronic diseases: Conditions such as kidney failure, gout, and thyroid disease can lead to nerve damage.
- Blood protein disorders and cancers: Multiple myeloma and other blood cancers can cause an abnormal buildup of proteins known as paraproteinemia that can damage nerves or the blood vessels that supply the nerves.
What Are the Types of Peripheral Neuropathy?
There are many different types of PN. It is classified in numerous ways, including by the nerves affected, underlying causes, and symptom characteristics. Some of the ways PN can be classified include the following:
Distribution
- Mononeuropathy: affects a single nerve
- Polyneuropathy: affects multiple nerves
- Multiple mononeuropathy: affects two or more nerves in different areas
Nerve Fibers Affected
- Large fiber neuropathy: affects large, myelinated nerve fibers
- Small fiber neuropathy: affects small, unmyelinated nerve fibers
- Mixed fiber neuropathy: affects both large and small fibers
Function
- Motor neuropathy: affects nerves controlling muscles
- Sensory neuropathy: affects nerves transmitting sensory information
- Autonomic neuropathy: affects nerves controlling involuntary functions
- Sensorimotor neuropathy: a combination of sensory and motor nerve involvement
Cause
- Acquired neuropathy: caused by environmental factors, illnesses, infections, etc.
- Hereditary neuropathy: caused by genetics
- Idiopathic neuropathy: cause unknown
Who Is at Risk of Peripheral Neuropathy?
PN risk is influenced by various factors, some of which cannot be changed (unmodifiable) and others that can potentially be controlled through lifestyle choices (modifiable). Factors that increase the risk of developing PN include the following:
- Age: The risk of PN increases with age. In the general U.S. population, the prevalence is about 10.4 percent in those aged 40 to 69 and 26.8 percent to 39.2 percent for older adults. While some hereditary neuropathies, like CMT, may appear in childhood, other inherited neuropathies may develop in adulthood.
- Sex: Males have a much higher likelihood than females of developing PN, but females are more likely to experience pain.
- Race: PN is more common among black people than white.
- Height: Taller people are considerably more likely to develop PN, likely due to the longer length of their nerves.
- Genetics: Some sources of neuropathy, like CMT, familial amyloidosis, and Fabry disease, can be inherited.
- Diabetes and metabolic conditions: Prediabetes or diabetes substantially increases the risk of developing PN. The prevalence of PN is more than twice as high in adults aged 40 to 69 years with diabetes compared to those without diabetes. The risk increases with the duration of the disease, with more than half of diabetics likely to develop the condition.
- Body mass index (BMI): A higher BMI, calculated as weight (in kilograms) divided by height squared (in meters), is a risk factor for developing PN.
- Education: Research shows that those with less education may have higher odds of developing PN.
- Smoking: Many—but not all—studies indicate a higher risk of PN is associated with smoking.
- Circulatory diseases: Conditions affecting the heart, blood vessels, and circulation can increase the risk of PN. Cardiovascular disease affects the heart and blood vessels, influencing overall circulation. A family history of cardiovascular disease also increases the risk of developing PN.
How Is Peripheral Neuropathy Diagnosed?
Early diagnosis, identifying the cause, and ruling out other conditions is key to effective treatment. Diagnosing PN takes a step-wise approach.
Step 1: Clinical Evaluation
In the first step, symptoms are assessed, and a detailed history is taken to obtain information about alcohol use, family history of neuropathy, recent illnesses or vaccinations, and use of neurotoxic medications such as gout medications, antivirals, and chemotherapy. Additionally, information about blood transfusions, sexual history, and intravenous drug use is gathered to assess HIV and hepatitis C as potential causes.
Clinical and neurological examinations follow, evaluating muscle strength, reflexes, and sensitivity to temperature, light touch, position, and vibration. The practitioner will consider the onset and progression of PN, whether symptoms are symmetrical or asymmetrical, their location, and the nerves involved, providing clues to the underlying causes and type of neuropathy.
Urgent referral to a neurologist is warranted for individuals experiencing sudden, severe, or worsening symptoms to ensure prompt treatment. This is particularly critical for those showing nerve damage in multiple areas, unusual patterns, or having only motor or autonomic symptoms without sensory changes.
Absent indications of referral necessity, this initial assessment may lead to a clinical diagnosis of PN. However, even in diabetics, additional testing is essential to eliminate other potential coexisting causes.
Step 2: Laboratory Tests
Laboratory tests help identify contributing factors and rule out other conditions. Depending on the individual’s clinical presentation and diagnostic findings, blood tests may include:
- Complete blood count (CBC) to evaluate overall health and detect a variety of disorders
- Erythrocyte sedimentation rate (ESR) to detect inflammation
- Comprehensive metabolic panel (CMP) to assess blood glucose, hemoglobin A1c, kidney function, and liver function
- Thyroid function tests to check for thyroid disorders
- Vitamin B12 with methylmalonic acid and homocysteine to identify vitamin B12 deficiency and its potential impact
- Vitamin B6 to check for deficiencies or excess that may affect nerve function
- Protein immunofixation to detect abnormal proteins in the blood
- Various autoantibody tests to identify autoimmune conditions
- Vasculitis tests to detect inflammation of the blood vessels
- Tests for specific viruses and bacteria to rule out suspected infections that can cause neuropathy
- Heavy metals to check for toxic exposure
- Genetic tests to identify hereditary neuropathies
Some of these tests may be ordered by the primary care practitioner or a neurologist following referral.
Step 3: Electrodiagnostic and Medical Tests
If initial tests are inconclusive, symptoms are complex, or other health conditions are present, further testing or a neurologist referral may be necessary. A specialist can then conduct advanced tests to provide valuable insights into the extent and nature of nerve damage. These additional assessments may include:
- Nerve conduction study (NCS): This test measures the speed and strength of nerve signals using sensors placed on the skin. It is considered the gold standard for diagnosing DPN. NCS can exclude other conditions, identify affected nerves, distinguish between axonal (nerve fiber) and demyelinating (nerve covering) damage, and determine damage severity.
- Electromyography (EMG): This test measures the electrical activity of muscles by inserting a small needle into the muscle. EMG helps confirm a PN diagnosis and provides additional information that can complement the findings of the NCS.
- Sweat testing: Sudoscan and Neuropad are noninvasive tests that diagnose small fiber neuropathy and early autonomic dysfunction by assessing sweat gland activity. Sudoscan uses electrochemical reactions to measure sweat gland function on the palms and soles, while Neuropad involves a color-changing patch on the foot to indicate sweat production.
- Imaging: Peripheral nerve ultrasound, magnetic resonance imaging (MRI), and magnetic resonance neurography (MRN) can reveal injured and compressed nerves not accessible by NCS or EMG. MRI provides detailed images of the overall anatomy, while MRN offers more specialized and specific imaging of peripheral nerves, but it is not as widely available.
- Biopsy: Nerve or skin biopsies may be obtained and analyzed. A nerve biopsy may help assess possible immune-mediated or infectious neuropathies, while a skin biopsy is used to determine nerve fiber density.
- Examination of cerebral spinal fluid (CSF): If the suspected cause is infectious, inflammatory, vasculitic (related to blood vessel inflammation), or paraneoplastic (related to cancer), the CSF may be analyzed.
Other less common, newer, or not widely available tests include VibraTip, corneal confocal microscopy, laser-evoked potentials, and quantitative sensory testing.
What Are the Possible Complications of Peripheral Neuropathy?
While peripheral neuropathy is often a complication of other conditions, it can lead to its own set of complications due to nerve damage. These include:
- Injuries: Without sensations, sharp objects, heat, and extreme cold can cause unnoticed wounds.
- Falls: Nerve damage affects gait, coordination, and balance, increasing fall risk.
- Pain and hypersensitivity: Up to 24 percent of those with DPN experience pain affecting sleep and quality of life. Hypersensitivity, where unpainful stimuli cause pain, is also common. Even the light touch of bedsheets can be unbearable.
- Disability: Nerve damage can make daily tasks difficult or impossible.
- Foot ulcers and amputation: About 30 percent of diabetics develop foot ulcers during their lifetime, with a high risk of recurrence. They are serious complications that can go unnoticed due to nerve damage, leading to infections or gangrene. Poor circulation and high blood sugar hinder healing, with over half of ulcers becoming infected, often resulting in lower limb amputation.
- Autonomic dysfunction or failure: Damage to autonomic nerves can cause cardiovascular issues (irregular heart rate or blood pressure), digestive problems, difficulty swallowing, urinary issues (incontinence, frequent infections), and difficulty regulating body temperature.
While these complications can be serious, there are steps that patients and their families can take to prevent or manage some of them effectively and improve quality of life. Here are some practical strategies:
- Foot care: Inspect feet daily and immediately address foot injuries; wear clean, dry socks and closed-toed shoes.
- Driving safety: Regularly assess whether driving is safe.
- Fall prevention: Be aware of surroundings, install railings, remove throw rugs and trip hazards, and install nightlights.
- Burn prevention: Set the water heater at 125 degrees Fahrenheit or lower to avoid burns.
- Health checkups: Get regular checkups to help manage blood pressure, digestive issues, and body temperature regulation.
What Are the Treatments for Peripheral Neuropathy?
Treating PN can be complex due to its many underlying causes and symptoms. The primary goal is to address the identified cause, such as managing blood glucose in diabetics or correcting vitamin deficiencies. In about 20 percent of cases, no cause is identified. However, symptoms can still be treated to improve quality of life, according to studies in Norway and the Netherlands, as mentioned in a 2020 paper in Neurological Research and Practice.
Traditional painkillers are typically ineffective for nerve pain, so other medications are generally utilized. Unfortunately, these medications do not work for everyone; they do not address the underlying cause of PN and often come with significant side effects.
1. Anticonvulsants
Despite limited effectiveness and significant safety concerns, gabapentin is widely prescribed as a first-tier treatment for neuropathic pain. Some researchers recommend reconsidering its use. A Cochrane Review found that gabapentin provided over 50 percent pain relief to about 38 percent of people with painful DPN.
Safety concerns arise when gabapentin is taken with drugs like benzodiazepines and opioids. In a study of accidental mixed-drug deaths involving opioids, gabapentin was present in about 25 percent of cases. Adverse effects include daytime sleepiness, weight gain, edema, and dizziness, with additional concerns about cognitive impairment, dementia risk, addiction, abuse, misuse, and illegal distribution.
Another option is pregabalin. However, research shows that for the majority of people with painful DPN, pregabalin provides little relief. At a dosage of 300 milligrams, only one in 22 people experienced a reduction in pain of 50 percent or more.
2. Antidepressants
Antidepressants, such as tricyclic antidepressants (e.g., amitriptyline, nortriptyline) and serotonin-norepinephrine reuptake inhibitors (SNRIs) (e.g., duloxetine), are effective in treating neuropathic pain. Duloxetine has been shown to provide better pain relief than pregabalin. These medications work by increasing levels of norepinephrine and serotonin in the nervous system, which helps reduce pain signals. Be sure to discuss the potential side effects with your prescribing practitioner.
3. Analgesics
Controlled-release oxycodone has been found to be an effective treatment in painful DPN with significantly improved quality of life. Tramadol, tapentadol, and other opioids may also be effective and are sometimes prescribed for severe neurologic pain. However, they should be used cautiously due to the associated high risk of addiction, misuse, illegal distribution, and when used with coexisting severe psychiatric conditions.
4. Corticosteroids, Plasma Exchange, and Intravenous Immune Globulin
These treatments are used for severe neuropathies caused by inflammation or immune attacks on nerves, like chronic inflammatory demyelinating polyradiculoneuropathy (CIDP). Steroids reduce inflammation. Plasma exchange (PE) removes harmful antibodies from plasma and replaces it with a substitute solution. Intravenous immune globulin (IVIG), made from pooled antibodies from healthy donors, helps regulate the immune system.
5. Other
As for topical medication, lidocaine patches or capsaicin cream may provide localized relief with few systemic side effects.
Other potentially effective treatments include surgery for cases of nerve compression, transcutaneous electrical nerve stimulation (TENS), spinal cord stimulation (SCS), physical and occupational therapy, acupuncture, and low-level laser therapy.
Studies show that combining traditional Chinese medicine (TCM) with Western medicine can improve effectiveness and nerve function. Emerging therapies such as ARA 290, a peptide, are also being explored for potential benefits in managing PN associated with sarcoidosis.
How Does Mindset Affect Peripheral Neuropathy?
Peripheral neuropathy can significantly affect a person’s daily life, affecting mood, sleep, and overall quality of life. Chronic pain, numbness, and other symptoms associated with PN can lead to sleep disturbances, which in turn can exacerbate the perception of pain, creating a vicious cycle. Additionally, the financial burden of associated direct and indirect costs can create stress that further degrades quality of life.
While PN symptoms can influence mental state, mindset also plays a significant role in how individuals experience and manage their condition. A large study on various pain conditions found that certain thought patterns, such as thinking the worst about pain, fearing pain, and being overly aware of pain, are strongly linked to negative emotions, anxiety, depression, higher pain intensity, and greater interference with daily activities.
This research underscores the importance of addressing mindset in PN management. A positive mindset can be a powerful tool in coping with PN and potentially improving outcomes. Here are key aspects of how mindset influences PN:
- Pain perception: Research has shown that mindset can influence how the brain processes pain signals. A more positive outlook may help reduce the perceived intensity of pain.
- Fear: Fear of falling can lead to decreased physical activity, which causes muscle weakness and loss of balance, further reducing mobility. This inactivity creates a vicious cycle, increasing the risk of falls. Other fears can play a role in this cycle, such as the fear of not being taken seriously or the fear of becoming disabled. Addressing this fear through mindset techniques and building confidence in safe movement can improve both physical and mental health.
- Impact on physical health: The stress and anxiety resulting from fear can trigger the body’s “fight-or-flight” response, leading to increased cortisol levels. Chronic high cortisol levels can contribute to inflammation, suppress immune function, and impair healing processes. These physiological changes can exacerbate neuropathy symptoms and hinder recovery. Adopting stress-management techniques and maintaining a calm mindset can help mitigate some of the adverse effects of stress on nerve function.
- Treatment adherence: A proactive mindset can improve adherence to treatment plans, including medication regimens, physical therapy, and lifestyle modifications.
- Coping strategies: A resilient mindset can help individuals develop and implement effective coping strategies, leading to improved quality of life despite PN symptoms.
What Are the Natural Approaches to Peripheral Neuropathy?
While many people use natural and herbal remedies, scientific evidence supporting their effectiveness is often limited. What works for one person may not work for another. Natural products can cause adverse reactions, interact with medications, or be contraindicated with certain medical conditions. Consult your health care provider or pharmacist for personalized advice.
Natural approaches to peripheral neuropathy can complement conventional treatment effectively. The first step is to eliminate or minimize the causative agent. Before starting any necessary chemotherapy, optimizing nutritional status may help prevent PN or lessen its severity. Since nerves regenerate slowly and the body does not produce new nerves, patience is essential, especially with natural approaches, as damage can become irreversible over time. Below are some natural approaches backed by peer-reviewed research.
1. Exercise
Research demonstrates that aerobic exercise can improve symptoms of PN, whether performed alone or in combination with resistance or balance training. A minimum of three weekly sessions of activities such as walking, cycling, or swimming is recommended. Simple exercises, including leg stretches and balance movements, can also enhance nerve function and reduce pain. Regular exercise can potentially delay progression, improve symptoms, and, in some cases, even reverse symptoms. It can also enhance blood flow, reduce cellular damage, and stimulate nerve regeneration.
2. Gluten-Free Diet
A gluten-free diet (GFD) can effectively reduce neuropathic symptoms and improve quality of life in those with gluten neuropathy, a type of peripheral neuropathy linked to gluten sensitivity. A small study found that those who strictly followed a GFD experienced better pain management and overall health compared to those who continued eating gluten. Gluten is incompletely digested and can cause inflammation by increasing intestinal permeability, even in individuals without gluten sensitivity.
3. Health-Promoting Fatty Acids
Omega-3 fatty acids help reduce inflammation, regulate blood pressure, glucose tolerance, and nervous system development and function.
Eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA) are two important omega-3 fatty acids primarily found in fatty fish. EPA is known for its anti-inflammatory properties, while DHA is crucial for brain health. A small pilot study found that supplementing with 1,000 milligrams of DHA and 200 milligrams of EPA for three months helped reduce pain in DPN.
One study found that gamma-linolenic acid (GLA) was as effective as alpha-lipoic acid (ALA) in reducing pain, although ALA may work more quickly in those with better kidney function. It is found in borage, evening primrose, and blackcurrant seed oils.
4. Additional Nutritional Support
Research has shown that supplementing with certain vitamins, minerals, and other nutrients can improve symptoms and quality of life for those with peripheral neuropathy. These beneficial nutrients include:
- Vitamin E: This vitamin may reduce the occurrence and severity of chemotherapy-induced PN and synergize with pyrroloquinoline quinone (PQQ).
- Mitochondrial support: PQQ and Coenzyme Q10 (CoQ10) have been shown to support mitochondrial function. PQQ has neuroprotective properties and promotes nerve regeneration by increasing nerve growth factor synthesis. CoQ10 has antioxidant properties, potentially improving energy production and reducing oxidative stress.
- Vitamin D: This vitamin is essential for nerve health, with deficiency linked to an increased risk of DPN. Supplementation may improve symptoms.
- B-complex vitamins: These include B1 (thiamine), B12 (methylcobalamin), folate (methylfolate), and B6 (pyridoxal-5-phosphate).
- Benfotiamine: This is a synthetic form of vitamin B1 that is more effectively absorbed and better at raising thiamine levels in the body. It can potentially reduce nerve pain and improve function in diabetic neuropathy.
- Magnesium: Magnesium deficiency is common. The mineral is required for normal thiamine functions.
- Copper: A copper deficiency can cause symptoms similar to vitamin B12 deficiency, such as nerve damage and sensory issues. This may occur in someone with a history of bariatric surgery, multiple nutritional deficiencies, or high zinc exposure, such as from supplements or certain denture pastes.
- Antioxidants: Antioxidants fight free radicals and balance ROS. Glutathione and ascorbic acid (vitamin C) are well-known for enhancing nerve regeneration. Melatonin, another powerful antioxidant, protects nerve cells, reduces inflammation at injury sites, and stimulates the growth of new nerve fibers.
- Alpha-lipoic acid (ALA): Another antioxidant, ALA, given both intravenously and orally, can help reduce pain and improve quality of life in people with DPN. It is found in beef heart and kidney, tomatoes, spinach, and Brussels sprouts.
- N-acetylcysteine (NAC): A precursor to glutathione, this neuroprotective agent promotes nerve cell survival by stabilizing cell membranes and helping prevent cell death.
- Fibrinolytic enzymes: Bromelain (found in pineapple) and lumbrokinase may help reduce pain and inflammation, improve circulation, and support nerve healing. Lumbrokinase may help prevent excessive scar tissue formation and promote regeneration.
- Hypericum (St. John’s wort): This natural antidepressant has anti-inflammatory and neuroprotective effects and potential benefits in reducing neuropathic pain.
- L-glutamine: Oral supplementation may reduce the occurrence and severity of chemotherapy-induced peripheral neuropathy.
- Curcumin: This is a compound in turmeric that may reduce DPN severity and lower blood sugar levels, along with various other health benefits. Nano-curcumin, a highly absorbable form, has shown promise in studies.
Individual supplementation or a professional formulation may be necessary to achieve therapeutic doses. While most B vitamins are safe in high doses, excess vitamin B6 can damage nerves and induce or worsen neuropathy.
How Can I Prevent Peripheral Neuropathy?
Preventing peripheral neuropathy involves maintaining good metabolic, vascular, and nerve health. Just as the risk of peripheral neuropathy increases with each component of metabolic syndrome, the protective benefits increase with each healthy diet and lifestyle change. Here are some key strategies:
- Maintain good blood sugar control: This is essential for diabetics, but keeping blood glucose levels in check can prevent nerve damage in everyone.
- Exercise regularly: Movement is critical, so rather than stressing over which exercises to do, it may help to seek guidance from a professional to choose safe and appropriate activities. Even simply walking can make a significant difference.
- Follow a healthy diet: Consume a balanced diet rich in organic fruits and vegetables, naturally raised lean meats, and omega-3 fatty acids found in foods like wild-caught salmon.
- Ensure adequate nutrient intake: Obtain sufficient amounts of vitamins, minerals, and other essential nutrients through a balanced diet and supplementation as necessary. Consult a nutrition professional for assistance.
- Avoid toxic exposures: Eat organic foods to avoid pesticides and chemicals. Limit alcohol consumption and avoid smoking, as these can contribute to nerve damage.
- Manage other health conditions: Keep blood pressure under control and maintain a healthy weight.
- Avoid prolonged pressure on nerves: Be mindful of repetitive motions or prolonged positions that compress nerves.
- Manage stress: Practices like yoga, meditation, or deep breathing exercises can help manage stress, which may exacerbate neuropathy symptoms.
